Stem Cell Therapy: A New Hope for Alzheimer’s Disease and Dementia
Stem Cell Therapy: A New Hope for Alzheimer’s Disease and Dementia
Introduction
Alzheimer’s disease (AD) – the most common cause of dementia – is a progressive brain disorder that leads to memory loss and cognitive decline. Current treatments can only manage symptoms or slow the disease’s progression slightly; they do not repair the brain damage that occurs in Alzheimer’s (Frontiers in Neuroscience). This has driven scientists to explore new approaches. One promising avenue is stem cell therapy, which aims to protect and even restore brain cells. In simple terms, stem cells are special cells that can grow into different types of cells in the body. Researchers believe they could replace lost brain cells or help the brain heal itself. Below, we break down how stem cell therapy might benefit patients with Alzheimer’s and dementia, what studies have shown so far, how it compares to traditional treatments, and what the future may hold.
How Can Stem Cells Help Alzheimer’s and Dementia?
Stem cells act like the body’s own repair system. In the context of Alzheimer’s and other dementias, stem cell therapy could prevent, slow, or possibly reverse damage in several ways:
Replacing Lost Brain Cells: Alzheimer’s causes neurons (brain cells) to die off. Stem cells can transform into new neurons and help repopulate and regenerate neuronal circuits, potentially replacing cells that have been lost (PubMed). For example, neural stem cells (which naturally form new brain cells) might be used to grow healthy neurons that improve memory and thinking.
Reducing Harmful Inflammation: Alzheimer’s brains often have chronic inflammation that worsens damage. Stem cell therapy has been shown to reduce neuroinflammation – calming the overactive immune response in the brain (PubMed). This is important because inflammation contributes to the injury and death of neurons that lead to cognitive decline (PubMed). By dialing down inflammation, stem cells create a healthier environment for brain cells to survive.
Clearing Out Toxic Proteins: Alzheimer’s is characterized by abnormal proteins – amyloid plaques and tau tangles – that build up in the brain. Studies suggest stem cells can help eliminate these protein clumps or prevent them from accumulating
(PubMed) (PubMed). They may do this by releasing enzymes or signals that encourage the brain’s cleanup cells (microglia) to clear amyloid, and indeed experiments have shown transplanted stem cells reduce amyloid and tau levels in animal models (PubMed). Clearing these toxic proteins could slow down or halt the disease process.Supporting and Protecting Neurons: Stem cells secrete beneficial chemicals called neurotrophic factors that help neurons survive, grow, and function. This support can improve synaptic connections (communication between neurons) and even boost energy production in cells (mitochondrial function) (PubMed). In other words, stem cells act like “nurses” for sick neurons – they release growth factors that keep existing brain cells healthy for longer and improve overall brain cell function, which can translate into better cognitive function.
Encouraging New Brain Cell Growth (Neurogenesis): Some stem cells can stimulate the brain’s own stem cells to divide and form new neurons. This promotion of neurogenesis could help the brain form new connections and memories (PubMed). Essentially, stem cell therapy might rejuvenate certain parts of the brain by fostering the birth of new neurons and supporting blood vessels in the brain, improving blood flow and nutrient delivery (PubMed).
Through these mechanisms, stem cell therapy offers a multi-pronged approach – it doesn’t target just one aspect of Alzheimer’s, but can address cell loss, protein buildup, and inflammation all at once. This is a key advantage over many current drugs, which usually focus on a single target. By attacking the disease from multiple angles, stem cells could potentially slow or even partially reverse the progression of dementia symptoms.
What Do Studies and Clinical Trials Show So Far?
Research into stem cell therapy for Alzheimer’s is still in early stages, but findings so far are encouraging. Scientists have conducted many studies in the laboratory and in animal models, and a growing number of clinical trials in human patients. Here are some of the key findings:
In the Lab and Animal Studies: Laboratory experiments and animal studies have demonstrated that stem cell treatments can indeed have beneficial effects on Alzheimer’s-like disease. In mouse models of Alzheimer’s, injected stem cells were able to migrate to the brain, where they reduced amyloid plaque deposition and tau tangles, promoted new neuron growth (neurogenesis), and even improved memory function in the animals (Alzforum). In one study, stem cells reduced brain inflammation and released signals that prompted the brain’s own immune cells to clear out amyloid plaques (Alzforum). Similarly, studies in older rats have shown human stem cells can reach the brain, transform into functional nerve cells, and restore learning, memory, and motor function that had been impaired (PubMed). These preclinical results give researchers hope that stem cells might have a real restorative effect on the Alzheimer’s-damaged brain.
Early Clinical Trial Highlights: Initial trials in people with Alzheimer’s or dementia are small but provide valuable insights:
Safety and Feasibility: A Phase I clinical trial in nine patients with mild-to-moderate Alzheimer’s tested the safety of injecting mesenchymal stem cells (derived from umbilical cord blood) directly into the brain’s ventricles (fluid-filled spaces). The approach was found to be feasible and generally safe, with no serious adverse effects; the main side effect was a temporary fever after the injections (PubMed). This important first-in-human study confirmed that delivering stem cells into the brain is possible and tolerable in patients, paving the way for larger trials.
Cognitive Improvements in an Early Trial: In another study, researchers tried a less invasive method – using stem cell byproducts called exosomes as therapy. Exosomes are tiny vesicles released by stem cells that carry many of their beneficial signals. In a Phase I/II trial, patients with mild to moderate Alzheimer’s received exosomes from mesenchymal stem cells intranasally (through a nasal spray) twice a week for 12 weeks (PubMed). The results were promising: no significant adverse events were reported, and patients in the medium-dose group showed improved cognitive test scores after 3 months of treatment (PubMed). Specifically, their Alzheimer’s cognitive assessment scores improved (indicating better memory and thinking ability) compared to their baseline, suggesting a potential therapeutic effect. While this was a small trial without a placebo control, it showed that a stem-cell-derived therapy could safely improve certain cognitive measures in patients at least in the short term.
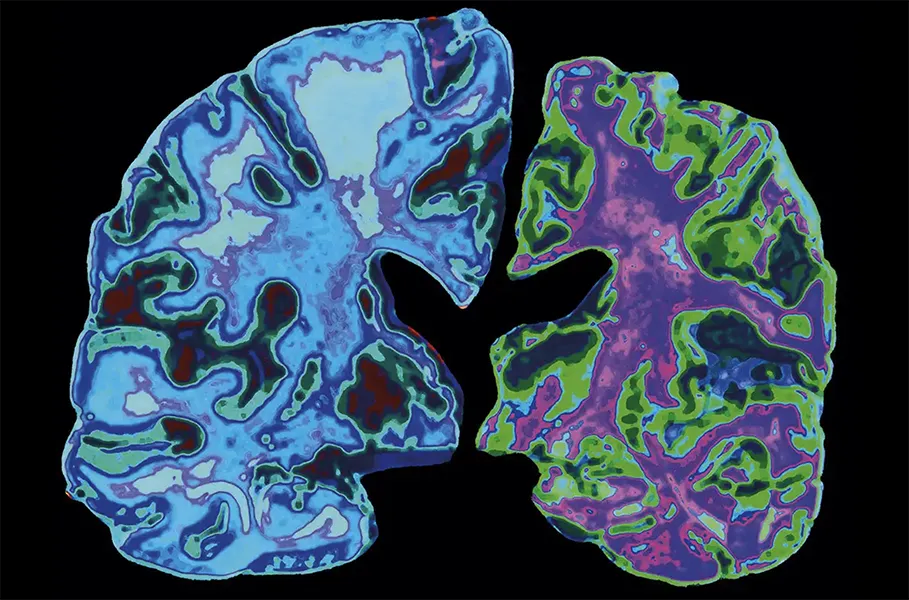
Intravenous Stem Cell Infusions (Lomecel-B): A U.S. biotech company tested an intravenous (IV) infusion of mesenchymal stem cells (product named Lomecel-B) in patients with Alzheimer’s. In a Phase I trial involving 32 patients, a single infusion of stem cells (at low or high dose) was compared to a placebo (Alzforum). The primary goal was to assess safety – and indeed, no major treatment-related side effects were observed (Alzforum). Though the study was small, researchers noted some encouraging trends: patients who received the stem cells showed reduced inflammation markers in their blood, signs of improved blood vessel function, and even a transient increase in hippocampal volume (the hippocampus is the brain’s memory center, which usually shrinks in Alzheimer’s) (Alzforum). Intriguingly, the low-dose stem cell group had a slightly slower cognitive decline over the next year compared to the placebo group (Alzforum). This suggests that even a one-time infusion might have some lasting beneficial effect. Building on these findings, a Phase IIa trial with multiple infusions was conducted in 2022–2023. Early results from that study indicated that the treatment remained safe (with no signs of brain swelling or micro-hemorrhages on MRI) and that the group receiving the lowest dose of repeated stem cell infusions actually showed a slight improvement in a composite Alzheimer’s score, whereas patients on placebo continued to decline (Alzforum). MRI scans also hinted that treated patients had slower brain shrinkage and lower signs of inflammation in the brain compared to those who didn’t get the stem cells (Alzforum). These findings, while preliminary, are exciting as they hint that stem cell therapy could modify the disease process, not just mask symptoms.
It’s important to emphasize that these studies are early-phase and involve relatively few patients. So far, the biggest takeaway is that stem cell treatments appear to be safe and achievable in human Alzheimer’s patients at least in the short term (PubMed). Many of the trials reported no serious adverse effects, which is reassuring for such an innovative therapy. In terms of effectiveness, the results show signals of benefit (like better cognitive scores or biological markers) but are not yet conclusive proof that stem cells work – larger and longer studies are needed to confirm these effects. Nonetheless, the fact that some patients showed stabilization or improvement in cognitive measures is something that almost never happens in Alzheimer’s with existing drugs, so these early signs are generating optimism among researchers and patients alike.
Stem Cells vs. Traditional Alzheimer’s Treatments
How does stem cell therapy compare to the treatments we already have for Alzheimer’s and dementia? The differences are significant:
Scope of Treatment: Traditional medications for Alzheimer’s (such as donepezil, rivastigmine, or memantine) mainly help with symptoms like memory loss or confusion. They do not stop the disease from progressing and they certainly cannot replace lost neurons. Even newer FDA-approved drugs that target amyloid plaques (like certain monoclonal antibodies) mostly slow the decline by a modest amount and come with risks (for example, brain swelling in some patients). In short, current treatments offer symptomatic relief or slight slowing, but no cure (Frontiers in Neuroscience). In contrast, stem cell therapy is aimed at altering the disease fundamentally – by regenerating brain tissue and restoring function, not just easing symptoms. Stem cells have the unique ability to become new brain cells and to modify the brain’s environment (reducing inflammation and toxic proteins), which means they could directly counteract the underlying damage of Alzheimer’s (Frontiers in Neuroscience). This regenerative approach is something no standard drug can do.
Disease Stage and Impact: Because conventional drugs don’t rebuild the brain, they tend to be most useful in early to mid stages of dementia to help maintain daily function a bit longer. Stem cell therapy, however, holds the potential to benefit even later stages by introducing new cells or protective factors to replace what’s been lost. For example, if a patient has lost a lot of cholinergic neurons (important for memory), no pill can bring those back – but a neural stem cell transplant might one day supply new cholinergic neurons to restore some function (PubMed). This could mean that stem cells, if proven effective, might actually improve cognitive function or slow disease progression in a way that current treatments cannot.
Targeting Multiple Pathways: Traditional treatments usually hit one target (for instance, increasing neurotransmitters or clearing amyloid). Alzheimer’s, however, is a complex disease involving many factors (cell death, protein aggregates, inflammation, etc.). Stem cells act more like a “multi-tool”, addressing several of these factors at once (PubMed). This multi-target approach could be more effective in a disease like dementia, which is why researchers are so interested – stem cells could combine the benefits of several drugs in one therapy by simultaneously protecting neurons, reducing plaques/tangles, and fostering repair (PubMed).
It’s worth noting that stem cell therapy for Alzheimer’s is not yet an established treatment – unlike the standard medications, it’s still experimental. So for now, traditional treatments remain the mainstay for managing Alzheimer’s symptoms, but they have clear limitations. Stem cells represent a completely different strategy that, if successful, might one day work alongside or even outperform traditional drugs in preserving brain function.
Future Research: What’s Next for Stem Cell Therapy?
The early successes in stem cell research for dementia are exciting, but many questions remain. Scientists are continuing to explore how best to harness stem cells to combat Alzheimer’s and related dementias. Here are some key areas of future research and what they mean for patients:
Larger and Longer Trials: The next step is conducting bigger clinical trials (Phase II and III) to truly test effectiveness. Ongoing studies are enrolling more patients and using placebo control groups to see if stem cell therapy can consistently slow cognitive decline or improve daily functioning. These trials will also track patients for a longer period to ensure that any benefits are sustained and to monitor for late-arising side effects (PubMed). It’s possible that if these larger trials show positive results, stem cell treatments could move toward FDA approval and wider use in the coming years. Until then, they remain available only in research settings (or special compassionate use cases).
Optimizing Treatment Methods: Researchers are investigating the best ways to deliver stem cell therapy. Is it more effective to inject cells directly into the brain, infuse them through an IV, or even give them as a nasal spray? Each method has pros and cons: direct brain injection places cells right where needed but is invasive; IV infusion is much simpler but fewer cells may reach the brain; intranasal delivery could target the brain via the olfactory nerves without surgery. Ongoing studies will compare these methods to determine which is safest and most effective at delivering benefits to patients’ brains. Similarly, scientists are studying different types of stem cells – from mesenchymal stem cells (often sourced from bone marrow or umbilical cord) to neural stem cells and induced pluripotent stem cells (iPSCs, which are patient’s own cells reprogrammed to a stem-like state). Each cell type has unique advantages, and future research will reveal which are most suitable for treating Alzheimer’s
(PubMed) (PubMed).Addressing Safety and Ethical Challenges: While stem cell therapy has been safe in trials so far, there are important challenges that researchers are working to overcome. One concern is the risk of immune rejection – if the stem cells come from a donor, the patient’s immune system might attack them. Another is the risk of tumor formation – especially with potent cells like embryonic stem cells or iPSCs, there is a possibility (if not fully controlled) that they could form tumors or grow in unwanted ways (PubMed). Future research is focusing on making stem cell therapy as safe as possible, for instance by using a patient’s own cells (to avoid rejection) or by pre-differentiating cells into neural cells before transplant (to reduce any tumor risk) (PubMed). Ethical issues surrounding sources of stem cells (like embryonic stem cells) are largely being addressed by the development of iPSC technology, which can create embryonic-like stem cells from adult tissues. Overall, continued vigilance in safety studies is crucial as this field progresses.
Enhancing Efficacy: Scientists are also experimenting with ways to boost the effectiveness of stem cells. This includes genetic engineering or pre-conditioning of cells to produce extra healing factors, combining stem cell therapy with other treatments (for example, giving neurotrophic (growth) factors or anti-amyloid drugs alongside stem cells to see if together they have a bigger impact), and even using cell-free approaches. The cell-free approach involves using the healing molecules produced by stem cells (like the exosomes mentioned earlier) rather than the cells themselves. This could sidestep some risks and logistical issues of cell therapy. Early trials with exosomes have shown promise, and further research will likely expand on this strategy (PubMed) (PubMed). Another futuristic idea is precision medicine – customizing stem cell treatments for each patient. For instance, a patient’s own skin cells could be turned into iPSC-derived neural cells and then implanted back, tailoring the therapy to the individual. These innovations are on the horizon and represent the next chapter of stem cell research (PubMed).
In summary, the future of stem cell therapy for Alzheimer’s and dementia will involve careful refinement of the treatment to maximize benefits and minimize risks. The scientific community is cautiously optimistic: if ongoing studies confirm that stem cells can safely improve outcomes in Alzheimer’s, this therapy could revolutionize how we treat dementia. It might take several more years and further breakthroughs, but the momentum in research is strong.
Conclusion
Stem cell therapy is offering a beacon of hope in the fight against Alzheimer’s disease and other dementias. Unlike traditional therapies that only treat symptoms, stem cells aim to heal the brain itself by replacing lost cells and providing support to damaged areas. Early research indicates they can reduce the hallmarks of Alzheimer’s (like plaques, tangles, and inflammation) and possibly slow cognitive decline (Alzforum) (Alzforum). Clinical trials to date have shown that stem cell treatments are feasible and generally safe for patients, which is a crucial first step (PubMed). While it’s too soon to say that stem cells are a proven treatment, each new study brings us closer to understanding their full potential. In the coming years, results from larger trials will tell us just how effective stem cell therapy can be in improving memory and quality of life for those with Alzheimer’s. If the outcomes continue to be positive, we could be looking at a future where Alzheimer’s is no longer seen as irreversible – a future where regeneration and repair of the brain become part of the standard care. For now, patients and families can remain hopeful as science moves forward, and they can keep informed by following the latest research. Stem cell therapy for dementia is a story in progress, and it’s one that holds the promise of changing countless lives for the better (PubMed).
References and Further Reading:
For readers interested in the scientific studies behind these findings, here are links to some key research articles and reviews:
Liu et al. (2020). Stem cell therapy for Alzheimer's disease. Neural Regeneration Research, 15(8):1467-1476 – A comprehensive review of how various types of stem cells could be used to treat AD, summarizing preclinical results and clinical trial progress: https://pmc.ncbi.nlm.nih.gov/articles/PMC7477654/
Duan et al. (2023). Stem Cell Therapy for Alzheimer’s Disease: A Scoping Review 2017–2022. Stem Cell Research & Therapy, 14(1): 45 – A recent review highlighting the advantages of stem cells over drug therapies and outlining findings from recent studies (cellular, animal, and clinical levels): https://pmc.ncbi.nlm.nih.gov/articles/PMC9855936/
Kim et al. (2022). Intracerebroventricular injection of human umbilical cord blood mesenchymal stem cells in patients with AD dementia: a phase I trial. Alzheimer’s Research & Therapy, 13: 65 – The first human trial injecting stem cells into the brains of Alzheimer’s patients, demonstrating safety and setting the stage for efficacy trials: https://pmc.ncbi.nlm.nih.gov/articles/PMC8439008/
Xie et al. (2023). Clinical safety and efficacy of human adipose MSC-derived exosomes in patients with Alzheimer’s: a phase I/II trial. General Psychiatry, 36(5): e101143 – An innovative study using stem cell exosomes delivered intranasally, showing no adverse events and cognitive improvements at 12 weeks: https://pubmed.ncbi.nlm.nih.gov/37859748/
Lomecel-B Alzheimer’s Disease Trial Updates – AlzForum summary of results from Longeveron’s stem cell infusion trials (Phase I and IIa) This provides an easy-to-read overview of how an IV stem cell product performed in early clinical testing (hints of reduced inflammation, brain atrophy, and cognitive decline): https://www.alzforum.org/therapeutics/lomecel-b
Ullah et al. (2023). Neural Stem Cells in the Treatment of Alzheimer’s Disease: Current Status, Challenges, and Future Prospects. Cells, 12(16): 2048 – Discusses why neural stem cells are promising for AD, and delves into future directions and hurdles (like ensuring safety and choosing the best cell type): https://pmc.ncbi.nlm.nih.gov/articles/PMC10473082/
These resources offer more technical detail for those interested in the science behind stem cell therapy for Alzheimer’s. Each study adds a piece to the puzzle, and together they illustrate a hopeful trend: that regenerative medicine might one day change the outlook for neurodegenerative diseases like Alzheimer’s (PubMed).
